(Osteoarthritis and Degenerative Meniscus)
Core message: Mechanical loading through exercise drives cartilage health, pain modulation, and functional recovery; arthroscopy for degenerative tears offers little to no long‑term benefit.
Key evidence:
Moseley JB et al., N Engl J Med 2002;347(2):81‑88 — Placebo‑controlled trial showing no advantage of arthroscopic debridement or lavage over sham surgery.
Katz JN et al., N Engl J Med 2013;368(18):1675‑1684 — Meniscal tear with knee OA; no benefit of surgery compared to structured physical therapy.
Fransen M et al., JAMA 2015;314(21):2287‑2298 — Meta‑analysis confirming exercise as first‑line therapy with significant functional and pain improvements comparable to intra‑articular interventions.
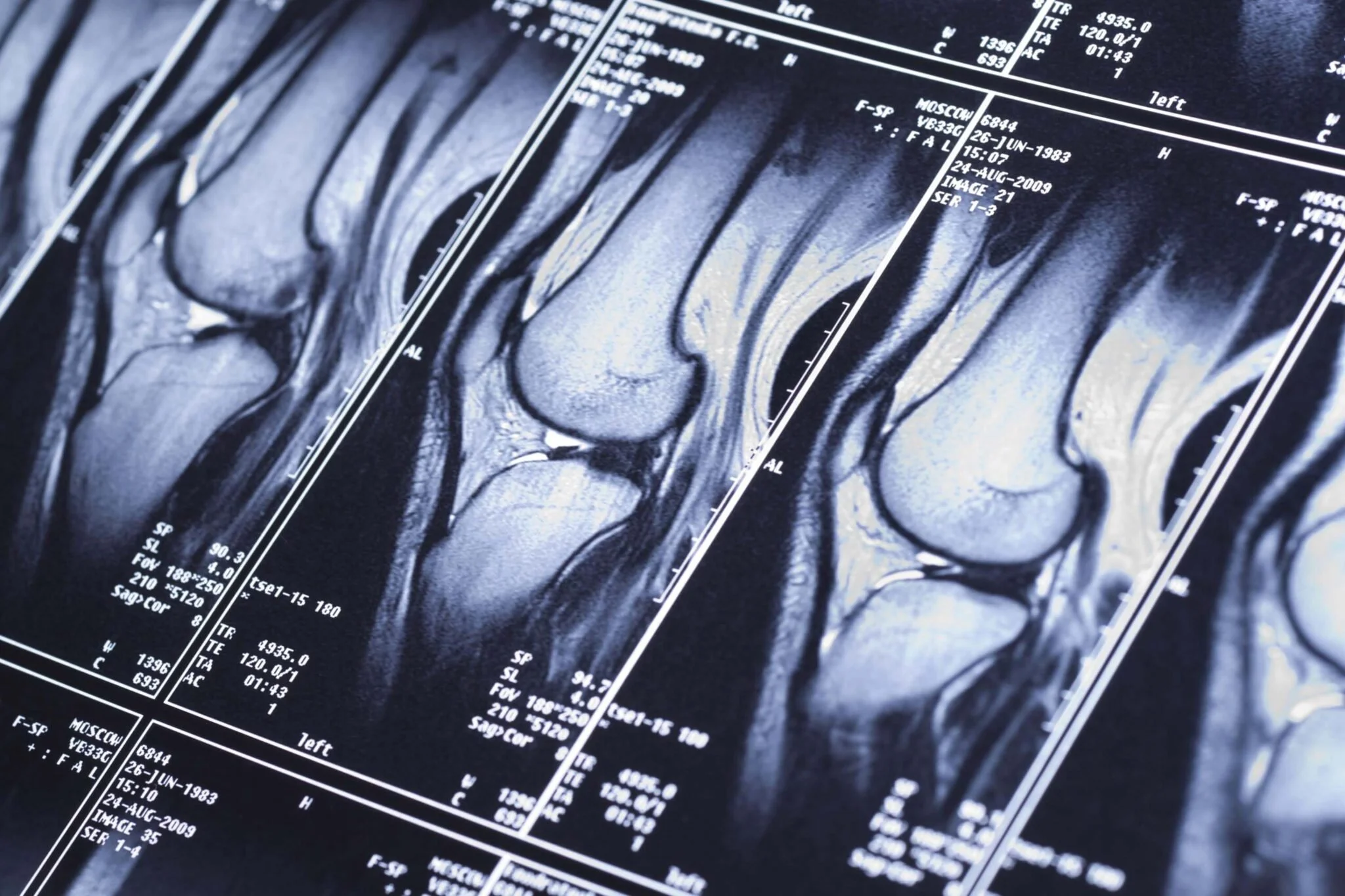
Knee
Osteoarthritis and Meniscal Injury
Clinical Layer:
OA and degenerative meniscus injuries benefit most from exercise and load-based interventions; arthroscopy rarely improves long-term outcomes.
Chronotherapy with physical and pharmacological agents improves results—timing matters.
Chronobiological Layer:
Aberrant rest/activity circadian rhythms are seen in OA and insomnia, linked with worse pain and recovery.
Cartilage chondrocytes possess a functional circadian clock modulating synthesis and matrix turnover; optimal joint activity timing enhances exchange and supports tissue repair.
OA pain itself follows a daily rhythm, peaking at certain times—treatment tailored to circadian phase may improve outcomes.
Why Should I Care?:
Knee cartilage repairs itself most efficiently at specific times. Exercising and recovering in sync with your daily rhythm increases repair and reduces pain, even for advanced arthritis.