Hip
(Osteoarthritis and Femoroacetabular Impingement Spectrum)
Core message: Targeted exercise and load management enhance hip stability, improve joint mechanics, and delay or prevent surgical intervention.
Key evidence:
Bennell KL et al., Ann Rheum Dis 2014;73(8):1451‑1457 — Physiotherapist‑led exercise improved pain and function in hip OA.
Wall PD et al., BMJ 2020;370:m3304 — Systematic review: exercise and education provide outcomes comparable to arthroscopic surgery for femoroacetabular impingement syndrome.
French HP et al., Arthritis Care Res 2013;65(7):1215‑1223 — Exercise therapy recommended as core management across OA stages.
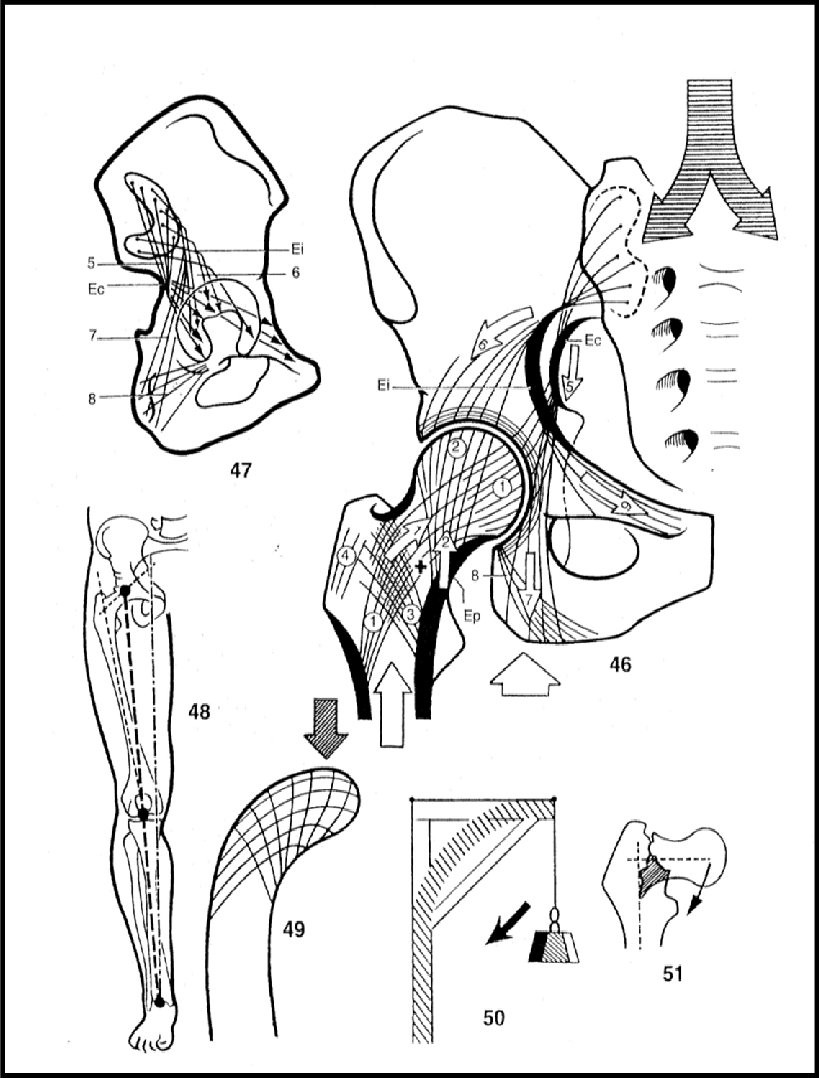
Hip: Osteoarthritis
Clinical Layer:
Structured rehab and exercise slow OA progression and delay the need for surgery. Exercise is the main intervention for pain and function, independent of imaging severity.
Circadian alignment of pharmacology and activity enhances joint outcomes.
Chronobiological Layer:
Hip osteocytes and chondrocytes are governed by local tissue clocks. Hormonal rhythms (cortisol, melatonin) further affect bone turnover and matrix integrity.
Nighttime rest and rehydration permit maximal ECM repair—misalignment results in degraded tissue quality.
Why Should I Care?:
Your hip heals best when your activity and recovery fit your body’s natural rhythm. Optimal exercise and good sleep together support the tissue clock, enabling better healing than exercise alone.